Statement of
Tammy Barlet, Associate Director
National Legislative Service
Veterans of Foreign Wars of the United States
Before the
United States House Of Representatives
Committee on Veterans’ Affairs
Subcommittee on Technology Modernization
and Subcommittee on Health
With Respect To
“VA Telehealth During the COVID-19 Pandemic: Expansion and Impact”
Washington, D.C.
Chairwoman Lee, Ranking Member Banks, Chairwoman Brownley, Ranking Member Dunn, and members of the subcommittees, on behalf of the men and women of the Veterans of Foreign Wars of the United States (VFW) and its Auxiliary, thank you for the opportunity to add recommendations on the expansion and impact of Department of Veterans Affairs (VA) telehealth during the COVID-19 pandemic.
Since the implementation of the VA MISSION Act of 2018, VA’s telehealth program expanded to connect veterans with their health care providers regardless of state lines. VA offers options for care through telehealth services at home, in the clinic, or in the hospital. Telehealth technology ranges from one-on-one visits to remote monitoring of health data like blood pressure, glucose levels, and weight management. According to VA’s official website over 900,000 veterans received care through VA telehealth in 2019.
The COVID-19 pandemic changed the dynamic of the American health care system. As Veterans Health Administration facilities and other health care systems throughout the nation applied a public health response, health care providers converted patient appointments to communication through telephone or video. Telehealth is playing a critical role in maintaining veterans’ mental and physical well-being during a time of social distancing and quarantine. During the pandemic, the need for telehealth expanded.
The VFW COVID-19 Survey
At the end of April 2020, the VFW released a survey to determine the experiences of veterans seeking to access VA health care, non-VA health care (private provider) and COVID-19 care since March 13, 2020. The survey also asked for a physical and mental health self-assessment during the past 30 days. Of the 7,153 survey respondents, 97% were military active duty, National Guard or Reserve, veterans, and retirees.
The survey objective for the sections of VA health care and non-VA health care was to gauge the transition of in-person routine care and critical/essential care appointments to telehealth when appropriate, and to determine how medication refills were handled since the President’s declaration of a national emergency on March 13, 2020. In addition, the survey asked how the individuals contacted their VA providers to facilitate care, and the satisfaction level of how their care was handled.
Most veteran respondents reported they continue to telephone VA to facilitate their care. The survey concluded that 52% of respondents called VA, while 32% used My HealtheVet secured messaging. The My HealtheVet platform allows veterans and certain eligible dependents, such as caregivers, to communicate with VA health care providers through secured messaging, refill prescriptions, schedule appointments, and access VA lab and test results. Again, according to the official VA website, My HealtheVet had over 3.7 million active users with a 77% user satisfaction rate during the first quarter of 2020. The VFW urges VA to continue outreach to promote its ease of usage and access to secured messaging, prescription refills, and appointment scheduling, and to maintain the highest degree of cybersecurity to ensure user information is protected.
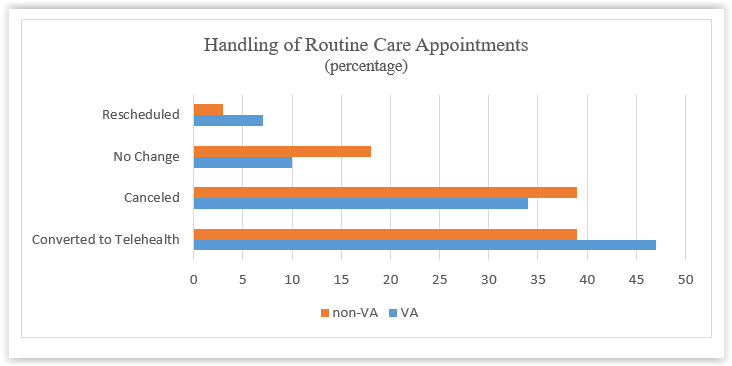
Shortly before March 13, 2020, VA instructed veterans with previously scheduled care appointments to contact their facilities. The VFW survey asked respondents how their routine care appointments with VA or non-VA providers were handled after March 13. VFW respondents reported that a majority 47% of VA routine care appointments were converted to telehealth, 34% percent were canceled, 10% were unchanged, and 7% were rescheduled. Most non-VA appointments, 34%, were either converted to telehealth or canceled, 33% were unchanged, and 3% were rescheduled. According to our survey data, VA converted more appointments to telehealth and canceled fewer appointments than non-VA providers. Also, non-VA providers were more likely to keep physical appointments than VA, potentially increasing veterans’ exposure to COVID-19.
 |
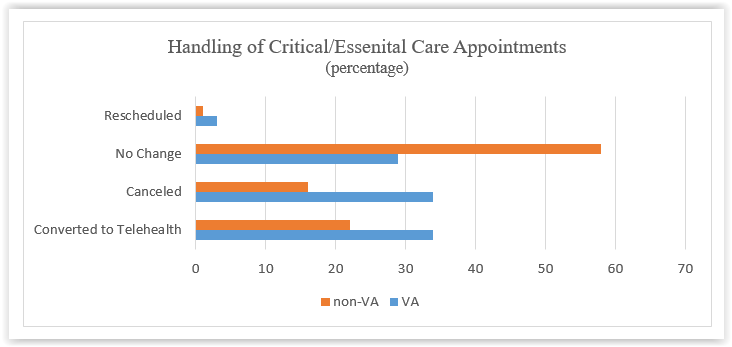
Not all appointments are routine care that can be postponed, rescheduled, or easily converted to telehealth. Critical/essential care appointments, such as cancer treatment, dialysis, cardiovascular intervention, or rehabilitative therapies, require in-person treatments, and pose substantial risk to the patient if they are delayed or canceled. After March 13, non-VA facilities were twice as likely to keep in-person critical/essential care appointments, and were less likely to reschedule those appointments than VA. Thirty-four percent of VA critical/essential care appointments were equally converted to telehealth or canceled, 29% were unchanged, and 3% were rescheduled. A majority, 58%, of non-VA critical/essential appointments remained unchanged, 22% converted to telehealth, 16% were canceled, and 1% were rescheduled. The vast difference between non-VA and VA critical/essential care appointments raises questions over the procedures for these appointments during the pandemic, such as the safety of both veterans and health care professionals.
 |
With the majority of both VA and non-VA appointments converted to a telehealth platform, medication refills remain a vital component to veterans’ health regimens. The VFW survey concluded that 90-92% of veterans expressed no changes with the handling of their medication refills through VA or non-VA, respectively. In addition, less than 7% of medications were delayed and less than 2% of medications were reported as unavailable. Therefore, the VFW believes that satisfactory communication with health care providers seemed to continue throughout the beginning stages of the pandemic, ensuring veterans continued to receive their necessary medication in a timely manner.Due to social distancing requirements, quarantining, and the abrupt change to how health care appointments are conducted, veterans reported that they adapted quickly to telehealth. According to the VFW survey, 59-62% of veterans were either satisfied or very satisfied with the care they received from both VA and non-VA health care providers. During a recent House Committee on Veterans’ Affairs hearing, VHA reported an increase in telehealth satisfaction levels since March 2020.
Telehealth Support
Over the years, the VFW has continuously supported telehealth expansion as a way to efficiently connect veterans to the health care services they need, specifically for mental health, veterans living in rural areas. and veterans who cannot easily travel to VA care facilities. A recent article in VFW Magazine discussed a study focused on providing a telehealth brain wellness program to a group of rural veterans with anxiety, depression, and PTSD. The VFW supports VA providing evidence-based telehealth programs by advocating for legislation and outreach.
Congress has moved VA forward in using telehealth as a tool to transform delivery of care to veterans. The passing of the VA MISSION Act of 2018 created a more convenient care option by allowing VA-licensed health care professionals to use telehealth at any location. This “anywhere to anywhere” approach allows veterans a continuum of care with providers they trust. However, there is more to be done. The option of telehealth also eases the fear of sexual harassment or abuse as veterans navigate their way through a VA medical center. Telehealth can eliminate extensive travel and wait times, which can remove geographic barriers or lessen the need to arrange for child care.
Through Project Advancing Telehealth through Local Access Stations (ATLAS), the VFW has worked with VA and Philips to leverage VA's anywhere to anywhere authority to expand telehealth options for veterans who live in rural areas. More than 20 VFW posts have been identified as possible telehealth centers, with plans to deploy five VFW ATLAS sites in the first phase of the program. The primary use for the first Project ATLAS site in Eureka, Montana, will be for mental health care, though the unique telehealth approach enables other kinds of health monitoring and consultation. Veterans in Eureka are required to travel more than 70 miles to the nearest VA clinic. Soon they will have the ability to receive VA health care closer to home. The VFW urges the House to incorporate the parts of S.785, Commander John Scott Hannon Veterans Mental Health Care Improvement Act of 2019, into the House companion bill, which would provide the opportunity to expand telehealth capabilities, and suicide prevention and mental health programs to veterans in rural and highly rural areas.
The VFW urges the House to pass H.R. 3228, VA Mission Telehealth Clarification Act, which would clarify the statute to include health professional trainees under the clinical supervision to provide treatment via telehealth. Many health professional trainees seek the opportunity to train in the nation’s largest health care system, and VA prides itself on offering an education with cutting-edge and innovative technology. The current statutory definition of covered health care professions includes residencies, internships, and students as outlined in Sections 7405 and 7406, in the VA MISSION Act of 2018, but these sections fail to mention that the health profession trainee is under the clinical supervision of a health professional while providing telehealth services. This is why the House must pass H.R. 3228.
Telehealth transformed both VA and non-VA health care systems to allow for continued access to care while social distancing and helping to flatten the curve of the COVID-19 pandemic. VA has utilized telehealth under federal law for many years, unlike certain federal and state programs which accelerated their flexibility and use of telehealth in response to COVID-19. To reach more veterans who may have been deterred from seeking VA care in the past, it is important to expand and support VA’s telehealth programs while continuing oversight.
The VFW understands the challenges VA endured since mid-March 2020 because of the COVID-19 pandemic. VFW membership is pleased and satisfied with the care they received via telehealth during the time of the stay-at-home order. The VFW would like to see telehealth continue to be offered as a tool to care for veterans.
This concludes my testimony. I thank you for the opportunity to testify and am prepared to answer any questions.
Information Required by Rule XI2(g)(4) of the House of Representatives
Pursuant to Rule XI2(g)(4) of the House of Representatives, the VFW has not received any federal grants in Fiscal Year 2020, nor has it received any federal grants in the two previous Fiscal Years.
The VFW has not received payments or contracts from any foreign governments in the current year or preceding two calendar years.