Statement of
Vincent “B. J.” Lawrence
Commander-in-Chief
Veterans of Foreign Wars of the United States
Before
Joint Hearing
Committees on Veterans’ Affairs
United States Senate and United States House of Representatives
Washington, D.C.
Chairmen Isakson and Takano, Ranking Members Tester and Roe, members of the Senate and House Committees on Veterans’ Affairs, it is my honor to be with you today with representatives of the more than 1.6 million members of the Veterans of Foreign Wars of the United States (VFW) and its Auxiliary –– America’s largest war veterans organization.
Blue Water Vietnam Veterans Act: The VFW thanks the committees for your devotion and hard work to ensure Blue Water Navy veterans finally receive the benefits they have been wrongfully denied for more than a decade. The VFW is glad to see the U.S. Court of Appeals for the Federal Circuit recently reversed a years-old ruling that potentially paves the way for the restoration of benefits for some 90,000 aptly named Blue Water Navy veterans from the Vietnam War.
The case, Procopio v. Wilkie, was supported by the VFW and a number of other veterans service organizations and advocates. It had Secretary of Veterans Affairs Robert L. Wilkie Jr. being sued by Navy veteran and VFW Life member Alfred Procopio Jr., who was denied service connection for prostate cancer and diabetes mellitus because he never stepped foot on dry land or served within Vietnam’s inland waterways. Mr. Procopio was assigned aboard the aircraft carrier USS Intrepid, which was stationed inside Vietnam’s 12-mile territorial waters. Both of his illnesses are listed among the Department of Veterans Affairs’ (VA) 14 presumptive diseases associated with exposure to Agent Orange.
The Federal Appeals Court focused on the intent of the 1991 Agent Orange Act, which was to grant a presumption of service connection for certain diseases to veterans who “served in the Republic of Vietnam.” At issue was whether service within territorial waters constituted service in the "Republic of Vietnam." By a 9-2 decision, the Appeals Court ruled it did.
While the VFW is pleased with the ruling, the decision can be appealed and overturned. Congress must pass H.R. 299, the Blue Water Navy Vietnam Veterans Act of 2019 to make certain Blue Water Navy veterans never have their benefits taken away again.
The Blue Water Navy Vietnam Veterans Act of 2019 also includes the extension of much needed benefits for Korean Demilitarized Zone (DMZ) and Thailand veterans. The VFW supports expansion of benefits for Korean DMZ veterans who suffer from diseases and illnesses directly linked to Agent Orange exposure. While many of these veterans receive presumptive disability compensation for their service-connected disabilities, hundreds of them are left out, despite clear congressional intent for them to be included. This legislation would provide them the benefits they have been unjustly denied.
This legislation would also provide benefits to children suffering from spina bifida because of their parents’ exposure to Agent Orange while serving in Thailand during the Vietnam War. Spina bifida is a debilitating birth defect, which has been found to be more prevalent among children of veterans exposed to Agent Orange. Children of Vietnam War and Korean DMZ veterans are eligible for this benefit, but children of veterans exposed to Agent Orange in Thailand are not provided the same support. This bill would make equal the level of benefits that other children receive due to their parents’ exposure to Agent Orange.
The 115th Congress failed to restore care and benefits for Blue Water Navy veterans because one senator did not believe Agent Orange made Blue Water Navy veterans sick and another senator was concerned about the cost. Congress cannot fail these veterans again.
MISSION Act Community Care: The VFW is proud to have work with Congress, VA and other veterans organizations for more than four years to analyze, improve, and build on lessons learned from the Veterans Choice Program. The VFW truly thanks committee members and staff for their hard work to shape and pass the VFW-supported VA MISSION Act of 2018. Now it is time to focus on the implementation of this multifaceted law. VA, Congress, and veterans organizations must work collaboratively to ensure it serves the intended purpose of improving the health care a grateful nation provides its veterans.
The VFW thanks VA for its quick implementation of the authority to provide veterans access to urgent care clinics in their communities. Doing so will fill the gap between emergency room care and outpatient care for veterans who do not have access to a VA medical facility in their area or are not able to be seen same-day at VA. However, the VFW strongly opposes the plan to charge veterans for service-connected urgent care. Any cost share associated with emergent or urgent care eligibility must be aligned with VA’s current copayment structure, which exempts veterans who do not have the financial means to afford copayments and veterans who receive care due to service-connected disabilities.
VA intends to waive copays for the first two urgent care visits. Additional visits would require a $30 copay. To the VFW, charging veterans for non-service-connected urgent care to deter over-reliance on more expensive urgent care instead of routine care is acceptable, but VA cannot charge for service-connected care, regardless of where such care is provided. Doing so would violate VA’s sacred mission to care for those who have borne the battle. VA must cover the full cost of caring for service-connected conditions, regardless of where such care is provided.
While the Veterans Choice Program has provided more than a million veterans with improved access to much needed health care, VFW members are looking forward to the day it is replaced with the new and improved VA Community Care Program. The VFW thanks the committee for the common sense and veteran-centric community care eligibility standards required by the VA MISSION Act of 2018. The VFW continues to believe that veterans must have access to care when and where they need it. The law established eligibility standards, such as when care is not available at VA or if community care is in the best medical interest of veterans, which accomplish that goal.
The law also grants VA broad authority to determine two of the six eligibility standards. One of those is access standards to replace the Veterans Choice Program’s arbitrary and confusing 30-day and 40-mile standards. While we are glad VA has finally published its plans for the access standards, we are disappointed VA chose not to incorporate the voice of our 1.6 million members in the decision-making process. As a result, VA is repeating previous mistakes. Twenty days is just as arbitrary as 30 days, and once again adopting TRICARE Prime Service Area standards is not in the best interest of veterans.
The VFW has provided substantive feedback and helped develop how America cares for her veterans since even before the Veterans Administration was created in 1930. VA executive leadership should be embarrassed that they have discounted VA’s collaborative relationship with the VFW and chosen to make arbitrary decisions without consulting with those who most intimately understand VA’s mission and the needs of the veterans community. We repeatedly asked for constructive discussion on access standards, only to be fed ridiculous excuses as to why they could not share what they were planning.
The VFW has made clear time and time again that VA must back away from setting arbitrary standards for when patients using VA are given the option to use community care. VA chose to ignore lessons learned from the Veterans Choice Program and recommendations from industry experts, such as the Transforming Health Care Scheduling and Access: Getting to Now independent review conducted by the National Academy of Medicine. VA must adopt standards that are tailored to the unique users of the VA health care system.
It is important for VA to establish access standards that define objective criteria for access to VA community care networks based on the needs of its unique system. The VA MISSION Act of 2018 provides VA the opportunities to do so by conducting Market Area Assessments, which must be used to align how and where VA provides health care to the needs and preferences of the veterans it serves. VA must establish standards that are sensible for VA’s capacity, and comparable to measures of local health care systems outside VA. Access and quality standards must balance the need to maintain the unique features of VA that effectually serve veterans, which cannot be reproduced in the private sector. While the VFW does not oppose VA’s proposed access standards, we feel VA missed an opportunity for veteran-centric reform. Instead, it chose to continue flawed wait time standards and readopt standards from the Military Health System, which serves a different population.
Continuing to base eligibility for community care on wait times is also counter to the peer-reviewed study published in the Journal of the American Medical Association. VA even lauded the findings of the study titled “Comparison of Wait Times for New Patients Between the Private Sector and United States Department of Veterans Affairs Medical Centers,” which found VA wait times have improved and outperform the private sector. The VFW was not surprised by the results of this study. VFW members report that the timeliness and quality of care they receive from VA continues to improve. The 20-day and 28-day eligibility standards are based on the false assumption that the private sector can meet the need when VA is unable to do so.
The success of the new community care program should be judged on how it improves health outcomes for veterans. Community care providers who wish to be part of the program must demonstrate a high level of expertise in veteran health, significant cultural competency about the veteran and military experience, and a commitment to improving and maintaining their skills and expertise.
The VFW also urges VA to account for how the implementation of a new electronic health care record impacts productivity. In partnership with the Defense Health Agency (DHA), the VFW has kept a keen eye on the implementation of the Military Health System GENESIS electronic health care record, which is the same system VA has elected to adopt for the VA health care system. While the VFW hopes VA adopts lessons learned from DHA to ensure a more seamless implementation, we are certain VA medical facilities will experience a temporary reduction in productivity that comes with change management. However, military treatment facilities report an eventual increase in productivity after full implementation. The VFW suspects VA medical facilities will experience a similar trend in productivity, which will lead to a temporary increase in demand for community care.
This and other temporary spikes in demand for community care, such as retirees who spend their winters in warmer climates, known are snowbirds, will require VA to adjust its community care networks and VA medical facility capacities to ensure veterans can receive the care they need where they need it. VA must make certain that temporary increases in demand for community care do not jeopardize the long-term viability of capacity at VA medical facilities. That is why the VFW urges VA and Congress to consistently evaluate whether VA should be expanding its community care networks or increasing internal capacity. This must be done by hiring more doctors or having VA deploy a quick reaction force of VA doctors to areas facing temporary spikes in demand for care.
VA facilities with service lines that fail to meet established quality standards will undergo remediation. Patients who rely on the 36 service lines that fall under the quality standards will have the opportunity to choose if they would rather stay with a VA doctor or use private sector doctors in their community. The VFW is disappointed VA chose not to include remediation plans in the recently published proposed rule. Remediation is vital to ensuring veterans get care based on their needs and preferences. VA must also take into account the ability for VA medical facilities to provide severely disabled veterans, such as those in spinal cord injury centers or polytrauma network sites, a full continuum of care. Simply closing such service lines in favor of community care would fail veterans who prefer to see a VA doctor and those who are unable to use community care. Allowing these decisions to be made by VA bureaucrats would be worse.
MISSION Act Staff Shortages: With nearly 50,000 vacancies, it is essential that Congress provides VA with the sufficient resources and tools to make it the preferred employer for medical professionals. The VA MISSION Act contains numerous provisions to strengthen, expand, and create new programs, including the VA Health Professional Scholarship Program; Education Debt Reduction Program; VA Specialty Education Loan Program; Veterans Healing Veterans Medical Access and Scholarship Program; Recruitment, Relocation, and Retention Bonuses; and Pilot Program on Graduate Medical Education and Residency. Additionally, the law expands VA’s authority to operate telehealth programs across state lines and requires VA to develop new health care programs specifically targeted to rural and underserved areas, both of which must remain priorities for VA. The VFW is proud to have partnered with VA and Philips to assist in expanding telehealth options for rural veterans as part of Project ATLAS. In this partnership, VA has identified highly rural areas where veterans must travel far distances to receive VA health care. The VFW identifies posts in those areas to serve as access points for VA health care. Once the post is modified to VA’s specifications, it is equipped with Philips-donated telehealth technology to provide veterans access to their VA health care at a convenient veteran-centric location. More than 20 VFW posts have been identified as possible telehealth centers. The VFW hopes this pilot is expanded to other communities.
Caregiver Program: With the passage of the VA MISSION Act, VA’s Program of Comprehensive Assistance for Family Caregivers (Caregiver Program) was finally expanded to include veterans who served before September 11, 2001. An estimated 76,000 veterans will enter the program –– an increase from the roughly 19,000 currently accessing these services. To avoid mishaps, VA must first ensure its administrative and IT capacity are prepared to manage an expanded caregiver program, followed by a two-phase expansion, beginning as early as 2019 for WWII to Vietnam War era veterans, followed two years later for post-Vietnam War veterans. The VA MISSION Act requires that an IT system be in place to properly manage and support the Program, avoid delays in access, and immediately identify resource needs. The law required such implementation to be no later than October 1, 2018. According to VA, it has implemented a permanent IT solution for current program participants. This system, however, is insufficient to support extending program eligibility, but VA is looking at other options.
Issues of insufficient resourcing and ineffective hiring processes for Caregiver Support Coordinators have significantly burdened the program. Congress must provide VA with sufficient resources for the management and staffing of this program. Without sufficient staff to respond to the needs of veterans, any efforts at successful expansion will be severely compromised. As noted by an August 2018 Office of Inspector General report, VA has not established a staffing model to ensure medical facilities are well-equipped to manage the current program’s workload, including processing applications and routine monitoring of veterans and caregivers. It is of utmost importance that VA has sufficient staffing numbers, and revises its program governance and workload to make this expansion a success. The VFW supports VA’s moratorium on discharges and decreased from the caregiver programs while it reviews and corrects these issues.
However, VA must take corrective action immediately so expansion of the program can proceed as soon as possible. Pre-9/11 veterans should not be forced forgo the choice of staying at home with their loved ones in lieu of inpatient long-term care simply because VA is to slow to fix issues it has know about for years.
As the regulations for the VA MISSION Act of 2018 continue to be drafted and published, the VFW will work to ensure VA properly implements the remaining sections of this important law. This includes working with VA and Congress to perfect billing, market assessments, expansion of the caregiver program, provider education and training programs, and the asset and infrastructure review.
Appeals Modernization: As a chief contributor to the development of the Appeals Modernization Act (AMA), the VFW is encouraged by VA’s efforts to seek congressional support and include stakeholders at multiple levels. Such collaboration demonstrates VA’s willingness and desire to improve the lives of veterans with innovative programs. As we have testified previously, we caution VA to heed the concerns and recommendations of those who represent a collective five million veterans in claims and appeals before VA. Often, the rush to implementation ends up being detrimental to those who are in need the most.
The process to overhaul appeals was lengthy, and involved disparate ideas and opinions. Negotiations were at times contentious, but it produced a product in which everyone involved has not just a stake but proprietorship. VA, to their credit, took all of these elements into account during development to make it something of value to help provide more timely benefits to veterans. We are also grateful that VA incorporated veterans service organizations’ concerns and expertise in crafting the federal regulations that now govern this new, modernized effort.
We have crossed the Rubicon –– the new appeals framework is now available to all veterans who disagree with their rating decisions. The VFW continues to support this new framework that offers veterans more options to resolve benefit disputes in a clear and timely manner. We believe that the system has the ability to work as intended, yielding positive results for veterans when the regulations VFW helped craft are applied impartially and as intended. VA should be applauded for deploying such substantial changes expeditiously. The VFW was eager to offer input and honest critiques as we navigate this new system together, and VA can expect continued oversight and input from us as we move forward with a modern system for modern times.
The VFW certainly understands the scope of the task at hand, which is why, in light of these successes, it is our obligation to call out potential problems in the system and work constructively with VA and these committees to make sure they are resolved. In our past testimony before the House Committee on Veterans’ Affairs, we highlighted three areas that needed improvement: informal conference through Higher Level Review (HLR), development errors at the VA Regional Office (VARO), and information technology (IT) infrastructure.
Now that the new framework is fully implemented, the VFW is concerned with the Board of Veterans Appeals’ (BVA) ability to handle its legacy appeals backlog, and interpret its own regulations on supplemental claim actions and veterans’ intent to file. Though VA assured Congress that it had a plan to address the legacy appeals backlog, we worry that VA is potentially setting itself up for failure through some of its recent actions.
More troubling is BVA’s inability to accurately certify legacy appeals. Before VSO representatives at the BVA can begin working on legacy appeals, the BVA must first. For years the VFW has been concerned about the number of legacy appeals waiting at the BVA just to be certified so we could begin our work. We have long called case storage at BVA appeals “purgatory.” This is where legacy appeals went to die and was one of the driving forces behind simplifying the process under AMA to directly certify appeals to the BVA.
In the past, appellants waited unreasonably long periods of time for their appeals to be certified at the VARO and activated by the BVA. We had no clear way to know exactly how many VFW-represented veterans had their appeals waiting in case storage. Unfortunately, in recent months, we have learned how bad the case storage backlog really was. Throughout 2018, the VFW would routinely receive between 300-500 new cases for our action each month. In January 2019, the BVA activated more than 1,900 new cases for the VFW. We feel this was done in haste to prepare for the new appeals process with no real assurance of accuracy. Such sloppy work and lack of quality control fails to identify the correct issues being appealed, and even leads to BVA erroneously assigning work to the wrong VSO. Coupled with the influx of appeals under the new framework, this is an unmanageable workflow for VSO staff stationed at the BVA, and does a disservice to the legacy appellants who have already waited years while the BVA sat on their claims. The BVA must correct this issue by improving its quality assurance and working with VSOs to develop and implement an effective strategy to address the legacy backlog.
Next, the VFW recently learned that VAROs are no longer accepting Intent to File (ITF) forms from veterans who seek to reopen previously denied claims years after a final decision was rendered. This is done to preserve the effective date of their claims when veterans do not have all the requisite documentation to file their claims. Their justification is that under AMA, veterans have recourse to continue benefit disputes indefinitely, but only if they meet the one-year filing deadline. While we certainly support the new framework whereby veterans have one year to continue claim actions and preserve their initial effective date, we believe that VA is misinterpreting the spirit of the AMA by not allowing ITFs after the expiration of the one-year appeal period.
VA explained that since the threshold to reopen a claim is now “new and relevant” as opposed to “new and material,” that veterans do not need as much time to develop reopened claims. The VFW disagrees. Moreover, how is the average veteran going to be able to delineate on future claims between reopened conditions, secondary conditions, new conditions, or increased conditions? VA’s current guidance is that veterans who wish to reopen after the one-year appeal period must still use the supplemental claim form, VA Form 21-0995. VA requires claimants to use VA Form 21-526EZ for any other claim actions, such as increases or secondary conditions. Requiring veterans to submit a supplemental claim form beyond the one-year appeal timeline is harmful for veterans and unmanageable for VSOs.
We compel VA to honor the ITF as a place holder for all future claims, including reopened claims, once the one-year appeal period has lapsed. We further compel VA to accept all future claims on the standard claim form, including reopened claims, once the one-year appeal period has lapsed. The VFW worries that this requirement will lead to veterans erroneously being denied benefits. The AMA was designed to simply the claims process for veterans.
AMA Informal Conferences: When the VFW last testified on Appeals Modernization, we called attention to significant inconsistency in how VA would schedule and conduct informal conferences for Higher Level Review claims. The VFW even commented on this provision through the Federal Register process. We pointed to examples in Seattle and St. Petersburg where Decision Review Officers (DROs) cold-called VFW representatives, and never offered the opportunity to schedule an informal conference.
The VFW’s understanding of the informal conference, as presented by VA, is that DROs should be reaching out to the party identified by the veteran on their HLR election to schedule a mutually agreeable time to conduct the conference. We did not see this happening consistently under RAMP. Instead, we saw that DROs were loosely interpreting VA’s requirement to make a “reasonable effort” to contact the VSO as any effort to contact any accredited representative, not necessarily the representative identified by the veteran in their election.
We have been assured by VA that this is not the standard for informal conferences. However, the lack of standardization across VA requires VSOs and Congress to strictly monitor this necessary component of appeals reform. VA must more clearly define reasonable effort, and provide explicit guidance on how reviewers will contact veterans’ designees to conduct informal conferences. While VA did not address this issue in the final AMA regulations, VA did adapt its forms and draft internal business processes to improve informal conferences. We have seen this situation improve and we believe that moving forward, VA will follow through on informal conferences keeping with congressional intent and the intent of the VSOs who requested this capability.
The VFW has seen very positive results for veterans when an informal conference is completed. This interaction is critical to the success of the AMA and ensuring that claim disputes are resolved at the lowest possible level, but it requires due diligence from VA.
AMA Information Technology Issues: When the VFW last testified on AMA, we expressed significant concerns on VA’s ability to deploy its required IT infrastructure on time. We see that VA was able to deploy the minimum requirements before the February 19, 2019, implementation deadline. This is a positive step, but one that must not be taken for granted.
In order to manage AMA, VA enlisted the help of U.S. Digital Service to create the Caseflow platform to track appeals. The VFW thanks VA for offering Caseflow access to all accredited VSOs when AMA was launched. However, much of our appeals work must still be completed through other systems, like the older Veterans Appeals Control and Locator System (VACOLS). We have been assured by VA that VACOLS will remain operational for the foreseeable future. However, we must keep a close eye on the further development of Caseflow to make sure that it functions properly for the tracking and processing of both legacy appeals and appeals filed after implementation of AMA.
It has been nearly 100 years since the VFW presented our first claims to the federal government for benefits for deserving veterans. The system has changed dramatically since 1919, and the VFW has been proud to be there every step of the way in building veteran-centric benefit programs. However, the VFW knows that changes to programs that were slow to mature last century move far more rapidly today. Training and oversight are key to the success of every VA business line. We have been given powerful tools to make the quality of life for veterans and their families better every day. Appeals modernization and the aggressive timelines it promises are going to be beneficial to many veterans, if they are implemented properly.
The VFW believes that VA is generally on the right track, since it has worked directly with stakeholders every step of the way to improve the process. We further believe that the roll out of the new appeals framework on February 19 was generally successful. However, we are not yet ready to declare the new framework a success, as veterans and VSOs are still stress testing the new system to see if it will fully function as intended. We look forward to working with VA and your committees to make sure the issues we discussed today are addressed and that the new appeals framework can deliver on its promise to veterans.
Poor Development at the VA Regional Offices: Another persistent problem is continued poor development of claims and appeals across VA, particularly at the VARO level, as the VFW has testified multiple times in recent months. Remand is a dirty word for veterans who have been waiting months for claims decisions and years for appeals to be heard. The AMA was developed with this in mind. Cases get entrapped in a vicious cycle of legal finger-pointing due to overlooked evidence, developers and raters overstepping their authority, or the general lack of responsibility. Lack of training and supervision lend themselves to this shortcoming.
While policies have been hashed out and best practices have been developed, the VFW worries that simply implementing the new appeals framework without addressing the broader training shortfalls in VA will only result in a rush to denial and more appeals being filed. We believe that VA shares this concern in some part. In conversations with VA, they have been candid that it does not anticipate a significant change in overall workload, but rather many veterans who are now waiting years for appeals in the legacy appeals system will request multiple avenues of recourse at lower levels through supplemental claims or higher level reviews.
Under the new framework, we believe that VA will be able to meet its objective of delivering supplemental rating decisions in a timely manner, but our goal is to help VA get it right the first time. That requires a greater commitment to the quality of work at the VARO level.
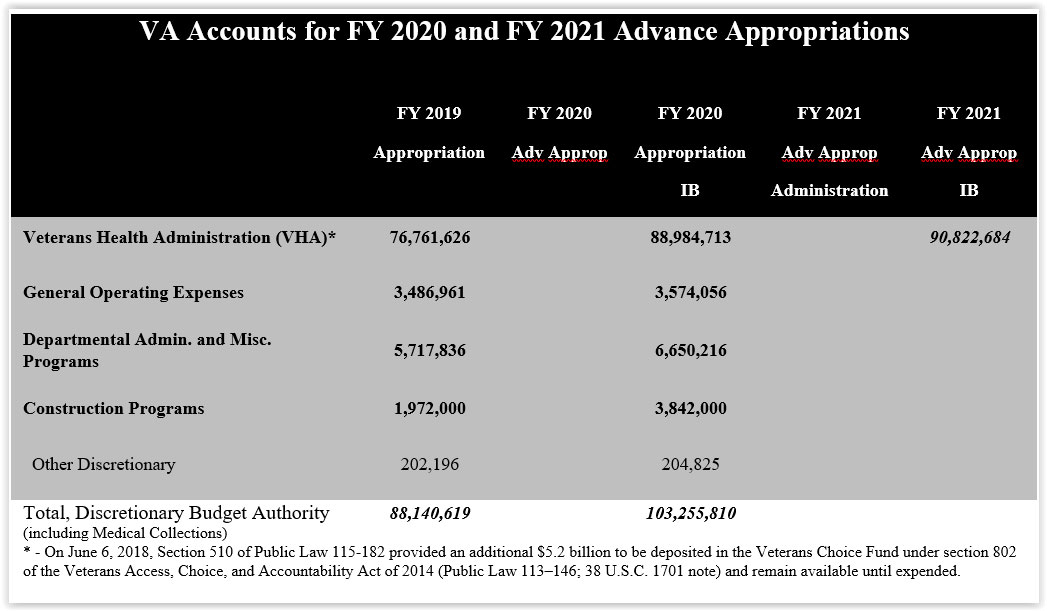
Fiscal Year 2020 Budget Request: The VFW, in partnership with the Independent Budget (IB), produces annual budget recommendations for each of VA’s major funding accounts and compares them to the Administration’s request. More complete details on the IB recommendations can be found at: www.independentbudget.org/:
The VFW was pleased to see the bipartisan budget agreement from this past year provided relief from the sequestration budget caps for veterans, service members and their families. Specifically, the agreement included $4 billion to address urgent VA infrastructure needs and increases the non-defense discretionary caps, which enabled VA to begin implementing its seamless VA Department of Defense (DOD) electronic health care record, fund the recent executive order to reduce the rate of suicide among recently discharged veterans, and improve access to health care for veterans.
Due in large part to landmark laws passed by these committees and the 115th Congress, VA will need a significant increase in appropriations for fiscal year 2020. This includes more than $9 billion for implementation of the VA MISSION Act of 2018. However, the bipartisan budget deal expires after fiscal year 2019, when sequestration spending caps, which were created in 2011, are set to be reinstated. Sequestration has already taken a massive toll on programs critical to our military and veterans. Congress must repeal the remaining sequestration spending caps and adopt a budget that meets our obligation to America’s service members, veterans, their families and survivors.
Medical Cannabis: VA must continue expanding research of non-traditional medical treatments, such as medical cannabis, for alternative therapies and less harmful ways of addressing health care issues for veterans within VA. VA must be proactive in finding solutions to responsibly treat veterans.
In the past several years post-traumatic stress disorder (PTSD) and traumatic brain injury (TBI) have been thrust into the forefront of the medical community and the general public in large part due to suicides and overmedication of veterans. Medical cannabis is currently legal in 33 states and the District of Columbia. This means veterans are able to legally obtain cannabis for medical purposes in over half the country. For veterans who use medical cannabis and are also VA patients, they are doing this without the medical understanding or proper guidance from their coordinators of care at VA. This is not to say VA providers are opting to ignore this medical treatment, but that there is currently a lack of federal research and understanding of how medical marijuana may or may not treat certain illnesses and injuries, and the way it interacts with other drugs.
This is regardless of the fact that many states have conducted research for mental health, chronic pain, and oncology at the state level. States that have legalized medical cannabis have also seen a 15-35 percent decrease in opioid overdose and abuse. There is currently substantial evidence from a comprehensive study by the National Academy of Sciences and the National Academic Press that concludes cannabinoids are effective for treating chronic pain, chemotherapy-induced nausea and vomiting, sleep disturbances related to obstructive sleep apnea, multiple sclerosis spasticity symptoms, and fibromyalgia –– all of which are prevalent in the veteran population.
The VFW urges Congress to pass legislation to require VA to conduct a federally funded study with veteran participants for medical cannabis. This study should include participants who have been diagnosed with PTSD, chronic pain, and oncology issues.
Women’s Health Care: VA reports that nearly 492,000 women veterans used the VA health care system in fiscal year 2017, which was a nearly 150 percent increase since fiscal year 2003, and these numbers will continue to increase in years to come. VA has worked to improve the gender-specific care for this population of veterans, but more work needs to be done. Women veterans using VA often have complex health care needs that require specialty care for service-connected conditions such as post-deployment readjustment challenges, PTSD due to war-related trauma and sexual trauma, mental health care, and substance use disorders — services which, on average, they use at higher rates and more often than male veterans. The VFW is disappointed not a single piece of legislation became law in the 115th Congress to address the needs of women veterans. This must change in the 116th Congress.
Peer-to-peer support has proven time and again to be invaluable to veterans and VA. This is why the VFW advocates so strongly for the constant expansion of peer-to-peer support programs The VFW urges Congress to pass legislation to expand these programs for women veterans, providing them more peer and gender-based one-on-one assistance from others to whom they can relate and connect. This is extremely crucial in instances where a women may suffer from mental health conditions, but especially in instances where a female veteran is on the verge of homelessness. In a VFW survey of women veterans 38 percent of women who reported experiencing homelessness also have children. These women face unique barriers to overcoming homelessness, and frequently commented on the lack of people who actually understand those barriers. By providing peer-to-peer support for women with others who have gone through the same hardships, VA would provide a level of understanding and trust they desperately need. This is why the VFW also urges Congress to pass H.R. 840, or S. 319, the Access to Childcare Act. Which would provide access to childcare to veterans seeking employment training who have an income at or below their states poverty line. Doing this would serve as a way to attempt avoiding homelessness.
According to VA, the majority of women veterans are assigned to Designated Women’s Health Primary Care Providers (DWHP). VA and its Center for Women Veterans have worked to increase those numbers, and the VFW asks Congress to provide VA with the resources they need to continue expanding outreach for knowledge of and access to providers with necessary gender-specific specializations. Surveys conducted by the VFW have found women veterans overwhelmingly prefer to receive their health care from women primary care providers, and are more likely to be satisfied with their VA health care experience when they receive care from women providers. That is why the VFW has urged VA to allow women veterans to choose the gender of their provider when enrolling in health care.
While the DWHP program continues expanding and providing above-satisfactory care to patients, the VFW understands there is still a need for trained gynecologists within VA. Gynecology is a specialty that has traditionally been understaffed at VA medical facilities across the country. While some providers are able to provide certain procedures that gynecologists specialize in and are able to treat, it is important to increase the number of doctors trained in the specialization of gynecology.
For women veterans who rely on VA for postnatal care, the VFW urges Congress to extend the number of days which newborn care is covered by VA. Typically, in private sector health care, a new mother has a month to enroll her newborn child into an insurance program. Currently, VA only covers newborn care for seven days. One week of coverage is not enough to provide coverage if anything goes wrong –– even in the relatively common instance of false-positive newborn disease testing –– nor is it enough to ease the new mother of unnecessary stress.
The VFW urges Congress to pass S. 514, the Deborah Sampson Act, which would also expand newborn coverage for veterans who use VA while receiving maternity care. In addition to expanding this care, the legislation would provide many other improvements women veterans needs within VA. Some of these improvements including increased privacy for women’s clinics, addressing lacks in gender specific care, further research, improving access to benefits, legal assistance and more.
The VFW applauds VA and Congress for their work to provide more access to gender-specific health care providers for women veterans. While overall progress has been made, gender-specific mental health care is still lacking. In VFW surveys, women veterans have voiced concerns over what they view as a lack of gender-specific training for mental health care providers. Congress and VA must work to ensure every VA medical center has mental health care providers who are well trained in conditions such as postpartum depression and conditions that stem from menopause or sexual trauma.
Women service members and veterans have also been found to be at increased risk for eating disorders, which have serious consequences for both physical and psychological health as well as high mortality rates. Some of the risk factors which contribute to women veterans struggling with eating disorders include military sexual trauma and combat exposure. As VA continues toward meeting the demands and needs of women veterans, it is important VA establish a comprehensive program for treatment of eating disorders.
The VFW has noticed a much lower utilization and awareness of benefits among older women veterans compared to their younger counterparts. In one of the VFW’s surveys, we found older women veterans were less likely to report receiving disability compensation, but equally as likely to have been injured or made ill as a result of their military service. Similarly, older veterans were less likely to report that they use VA health care, but equally as likely to report being eligible for VA health care than their younger counterparts. We were also concerned that several respondents who reported being 55 years old or older believed they did not rate the same benefits as their male counterparts, which is an egregious misperception that must be addressed.
No veteran should be left to wonder what, if any, benefits they are eligible to receive. Furthermore, it must be clear that women veterans have earned the exact same benefits as their male counterparts. That is why the VFW urges Congress and VA to continue improving outreach to women veterans and conduct targeted outreach to older women veterans to ensure they are aware of all the benefits and services VA provides.
Mental Health and Suicide: Eliminating suicide among our nation’s veterans continues to be a top priority for the VFW. As VA and Congress have continued to prioritize veteran suicide prevention, VA in cooperation with other government agencies continues to release annual data regarding veteran suicide. In September 2018, VA released its most recent analysis of veteran suicide with data from 2016. This data is expected to begin being released on a quarterly basis. The most recent data found suicide has remained fairly consistent within the veteran community over recent years. An average of 20 veterans and service members die by suicide every day. While this number must be eradicated, it is worth noting that as the number of veteran suicides has remained consistent in recent years, non-veteran suicides have continued to increase.
One death by suicide is one too many. Congress must ensure sufficient resources are available and used for effective VA suicide prevention efforts, including to identify veterans at higher risk of suicide, to adopt new interventions, and to effectively treat those with previous suicide attempts. Programs such as the Veterans Crisis Line (VCL); the placement of suicide prevention coordinators at all VA medical centers (VAMC) and large outpatient facilities; integration of behavioral health into primary care, and joint campaigns between DOD and VA should be continued to aid in anti-stigma efforts, and to promote suicide prevention efforts alongside community partners like the VFW.
The Government Accountability Office (GAO) has identified several key barriers that deter veterans from seeking mental health care. These include stigma, lack of understanding or awareness of the potential for improvement, lack of child care or transportation, and work or family commitments. Early intervention and timely access to mental health care can greatly improve quality of life, promote recovery, prevent suicide, obviate long-term health consequences, and minimize the disabling effects of mental illness.
Over the past decade, the VA Office of Mental Health Services has developed a comprehensive set of services while seeing a significant increase in the number of veterans receiving care. VA provided specialty mental health services to 1.6 million veterans in fiscal year (FY) 2015. In 2016, the MyVA Access initiative was announced to address urgent health needs of veterans, with a plan to make same-day primary care and mental health services available at all VAMCs. From the beginning of FY 2016 through June 2017, VA completed over one million same-day appointments for more than 500,000 unique patients through the primary care mental health integration or regular mental health clinics.
Since 2012, VA has worked to increase staffing of new mental health providers. Despite these efforts, according to an annual Office of Inspector General (OIG) report determining Veterans Health Administration (VHA) staffing shortages, FY 2018 saw that the most frequent staffing shortage within VA is psychiatry and the fourth most frequent in psychology. Out of 141 facilities surveyed, 98 had a shortage for psychiatrists and 58 had a shortage for psychologists. By not adequately staffing VA, the capacity to serve veterans and provide the necessary access to mental health care needed by so many veterans will continue to be limited. Having a limited capacity cannot be sufficiently addressed by using community care programs. The VFW urges Congress to work with VA on hiring efforts, and to keep this staffing shortage in mind as hiring incentives from the VA MISSION Act are used.
Veterans who served in Iraq and Afghanistan require a significant proportion of VA specialized mental health services. Without an end date for the Global War on Terror, this cohort will continue to grow, as will the need for specialized mental health services. Alarmingly, VA’s annual suicide data report has continuously shown veterans ages 18-34 have the highest rates of suicide. These numbers have continuously risen over the past three years, which is particularly worrisome as 54 percent of post-9/11 veterans fall into this age range. Studies show post-9/11 veterans who leave the military are also at increased risk of suicide during their first three years after service.
The VFW is grateful to the current administration for issuing Executive Order 13822, which required VA, DOD, and Department of Homeland Security to coordinate an interagency plan to provide seamless access to mental health treatment and suicide prevention resources for veterans during their first year of transition from military service to civilian life.
Additional framework was built into the Joint Action Plan (JAP) to provide more support for veterans at increased risk for suicide. This includes using current algorithms already implemented to identify veterans within VA who are at the highest risk of suicide. The overall goals of the JAP, which are still being implemented, include better assurance that all new veterans know how to access VA services.
There are also provisions in the plan that call for increasing partnerships between VA and private sector providers. The VFW understands that at times there is a need for care to be supplemented from within the community, but also firmly believes non-VA providers must be held to an equally high standard of care. It is imperative that veterans recently leaving their military service are able to access knowledgeable, evidence-based care through VA. Current reports show the care provided outside VA is of lower quality, and these providers prescribe veterans opioids at higher rates.
The VFW is proud to have partnered with VA on our Mental Wellness Campaign, along with other community and corporate partners like Give an Hour, the Elizabeth Dole Foundation, One Mind, PatientsLikeMe, and Walgreens. Beginning in fall 2016, this outreach campaign was launched to raise awareness, foster community engagement, improve research and provide intervention for those affected by invisible injuries and emotional stress. Since launching this campaign more than 200 VFW posts and 13,000 volunteers have successfully reached 25,000 people through our annual Day to Change Direction, hosted in partnership with Give an Hour’s Campaign to Change Direction. This event consists of the VFW, VA, and other partners conducting community service, spending time educating veterans, their families, and people in the community about emotional distress. Participants learn the five signs of emotional suffering –– personality change, agitation, being withdrawn, poor self-care and hopelessness. VA also provides information about programs and opportunities for assistance from VA and local community partners.
Another population at increased risk of suicide are veterans who received other than honorable (OTH) discharges. Veterans with this particular discharge have rapidly increased in recent years, and mostly received these discharges for administrative purposes without any due process, rendering them without access to VA. With the goal of eliminating veteran suicide in mind, Congress authorized and VA expanded access to mental health care for veterans who received an OTH discharge in July 2017. At the end of FY 2018, just over 100 veterans had utilized this care. The VFW urges Congress to provide oversight of this program and to work with VA on outreach programs educating veterans of its availability. The VFW also urges VA to open eligibility for all health care to veterans with an OTH discharge.
Surveys conducted by the VFW show veterans prefer using VA for reasons such as continuum of care and cultural competency. VA must continue developing ways veterans may access mental health care. VA must continue expanding telehealth options for veterans seeking mental health who are in rural areas and may struggle to access any form of health care. It is also crucial VA provide telemental health for women, LGBT, and racial/ethnic minorities who face unique barriers such as travel difficulties, lack of access to childcare, or increased concern of stigmas. VA must also expand mental health programs beyond trauma. Veterans need access to these appointments for issues related to families and lifestyles, as well as gender-specific needs such as post-partum struggles or during menopause.
Along with traumatic brain injury (TBI), post-traumatic stress disorder (PTSD) is closely correlated with post-9/11 veterans. PTSD is the psychological impact of experiencing or witnessing something traumatic. Like TBI, the effects of PTSD can be of an acute nature where veterans recover, or they can be chronic, resulting in symptoms that veterans may have for the rest of their lives without proper treatment. Regrettably, multiple deployments with intense exposure to combat have put many veterans at high risk for developing chronic PTSD.
VA has trained thousands of clinicians in the evidence-based protocols proven to be effective in addressing PTSD — cognitive processing and prolonged exposure therapies. Yet, treatment becomes more challenging as more veterans come to VA struggling with comorbidities. Common comorbidities include PTSD, military sexual trauma (MST), or TBI with Substance Abuse Disorder (SUD) and chronic pain. Many affected individuals experience high levels of anxiety or depression and exhibit difficulty with self-regulation, judgment, and concentration. Diagnosis is further complicated by the fact that veterans often may have coexisting conditions of TBI and PTSD. Symptoms of PTSD may significantly impair veterans’ ability to re-engage with their community and put them at higher risk for developing SUD, or death by suicide.
Unfortunately, many veterans have more than one mental health disorder. Patients with more than one diagnosis are often among the most difficult to treat. Current estimates of the prevalence of coexisting PTSD and SUD vary, although most findings suggest significant portions of the population with PTSD also have SUD. Researchers from the VA National Center on PTSD cite a large epidemiologic study, finding almost half of those in the general population with lifetime PTSD also suffer from SUD. This is why it is incredibly important for VA providers to take the proper steps to prevent at risk veterans from self-medicating, while also responsibly treating patients with chronic pain.
VA has also taken steps to ensure it appropriately uses pharmaceutical treatments. Under the Opioid Safety Initiative (OSI), VA has reduced the number of patients to whom it prescribes opioids by more than 22 percent. Prescribed use of opioids for chronic pain management has unfortunately led to addiction to these drugs for many veterans, as well as for many other Americans. VA uses evidence-based clinical guidelines to manage pharmacological treatment of PTSD and SUD to ensure better health outcomes. However, many veterans report being abruptly taken off opioids which they have relied on for years to cope with their pain management, without receiving a proper treatment plan to transition them to alternative therapies. Doing so leads veterans to seek alternatives outside of VA or to self-medicate. Congress must provide oversight of VA’s opioid reduction efforts to ensure they are effective and serve the best interest of veterans.
Military Sexual Trauma: MST continues to be a problem within DOD for all active, reserve, and guard components and it affects service members and veterans of all backgrounds without regard to age, gender or race. Most survivors of MST are males, but women are disproportionately affected. While DOD continues to increase its efforts to reduce or eliminate sexual trauma within the military service, the number of service members affected by MST is slow to decline. Congress must ensure DOD and VA improve their collaborative effort in awareness, reporting, prevention, and response among both service members and veterans.
VA’s national screening program screens all patients enrolled in VA for MST. National data from this program reveals about one in four women, and one in 100 men, respond affirmatively to having experienced sexual trauma while serving their country. All veterans who screen positive are offered a referral for free MST related treatment, which notably does not trigger the VBA disability claims process. Previous years of VA data show growing numbers exceeding 100,000 veterans receive care for MST related treatment.
In FY 2017, 3,681 men and 8,080 women submitted claims to VBA for health problems related to MST. Of those claims, 55 percent of men’s and 42 percent of women’s claims were denied. This is why the VFW encourages Congress to hold oversight hearings on VA care related to MST and VBA’s process of handling MST claims. It can take many years for survivors to even acknowledge a trauma occurred, and sharing details with advocates and care providers can be extremely difficult. Survivors of sexual assault often report they feel retraumatized when they have to recount their experiences to disability compensation examiners. Therefore, we encourage VBA to employ the clinical and counseling expertise of sexual trauma experts within VHA or other specialized providers during the compensation examination phase.
Burn Pits: The use of open air burn pits in combat zones has caused invisible, but grave health complications for many service members, past and present. Particulate matter, polycyclic aromatic hydrocarbons, volatile organic compounds and dioxins –– the destructive compound found in Agent Orange –– and other harmful materials are all present in burn pits, creating clouds of hazardous chemical compounds that are unavoidable to those in close proximity.
While the VFW is glad to see that more than 140,000 veterans have enrolled in VA’s Airborne Hazards and Open Burn Pit Registry, we are concerned that the results of the National Academies of Science’s study on the burn pit registry have not been fully implemented. The VFW urges Congress pass the Burn Pit Registry Enhancement Act, which would require VA to act swiftly on recommendations from this important study.
For example, a similar registry operated by Burn Pit 360 allows the spouse or next-of-kin of registered veterans to report the cause of death for veterans. VA must add a similar feature to its registry to ensure VA is able to track trends. Other improvements include streamlining the registration process, updating duty locations based on records provided by the Department of Defense (DOD), and eliminating technical glitches to ensure veterans are able to register. Another concern the VFW hears from veterans is the lack of outreach from the registry. Veterans expect to receive notifications or updates from VA on current research and VA’s progress to identify and treat conditions associated with exposure to burn pits.
Much of a veteran’s long-term health is dependent on what happened while in the military. Burn pit exposure can cause problems while in service, and this information must be shared with VA to ensure proper care is given. The VFW has long advocated for better sharing of information to include the location of burn pits, types of materials burned in the pits, data collected by industrial hygienists regarding exposures, data collected from post-deployment health assessments, and all information associated with a medical retirement caused by health conditions related to burn pit exposures. That why the VFW supports the Burn Pits Accountability Act.
Such information from DOD will go a long way to make certain veterans receive the care and benefits they deserve. The VFW urges Congress to ensure VA and DOD finish developing the Individual Longitudinal Exposure Record, which is intended to track when and where service members are deployed and to which toxins they were exposed. This program will have a tremendous impact on our ability to identify, prevent, and treat harmful health conditions associated with exposure to burn pits and other toxins.
The National Academy of Medicine report on the VA’s Airborne Hazards and Open Burn Pit Registry noted that there was a connection between burn pit exposure and numerous health conditions including emphysema, chronic obstructive pulmonary disease (COPD), and asthma. A peer-reviewed study entitled New-onset Asthma Among Soldiers Serving in Iraq and Afghanistan, published in the Allergy & Asthma Proceeding and conducted by staff at the VA Medical Center in Northport, New York, also found a connection between deployment to Iraq and Afghanistan and asthma among the 6,200 veterans reviewed. Other studies have shown similar evidence of association between pulmonary conditions and exposure to toxic burn pits. While more research can and should be continued to be conducted, the VFW believes it is time to grant veterans benefits for pulmonary conditions, which we all know are associated with deployments to the wars in Iraq and Afghanistan.
Additionally, the National Academies of Sciences Engineering and Medicine found in its recent report entitled Gulf War and Health, Volume 11: Generational Health Effects of Service in the Gulf War, that certain birth defects and reproductive issues are associated with exposure to toxic substances and illnesses which are prevalent in Iraq and Afghanistan. It is vital that VA and Congress address this report and ensure the generational impacts of burn pits are not allowed to go unrecognized.
Fort McClellan: From 1943 until its closure in 1999, Fort McClellan, Alabama, was home to thousands of soldiers in the Women’s Army Corps, the Army’s Military Police Corps, and the Army’s Chemical Corps. It was forced to close in 1999 due to investigations by the Alabama Department of Public Health, the Alabama Department of Environmental Management, the Agency for Toxic Substances and Disease Registry, and the U.S. Environmental Protection Agency, which discovered evidence of polychlorinated biphenyls (PCB) contamination in Fort McClellan’s neighboring town, Anniston.
The VFW has heard from several veterans suffering from deteriorating health conditions consistent with PCB exposure that they are unable to obtain the care and benefits they need because their service at Fort McClellan is not considered presumptive exposure to toxic substances. The VFW calls on Congress and VA to devote more time and attention to the health effects associated with exposure to PCBs at Fort McClellan, and to ensure exposed veterans have access to the care and benefits they deserve.
Camp Lejeune: Thanks to efforts by members of these committees, VA is authorized to provide no-cost health care to veterans and their families for 15 health care conditions that have been found to be associated with exposure to contaminated water on Camp Lejeune. However, VA expanded presumptive disability compensation benefits for only eight of the 15 conditions. As a result, veterans who served 30 or more days at Camp Lejeune between 1953 and 1987 and have been diagnosed with esophageal cancer, breast cancer, renal toxicity, female infertility, lung cancer, hepatic steatosis, miscarriage, and neurobehavioral effects, are eligible for no-cost VA health care, but still have an uphill battle obtaining disability compensation benefits. The VFW urges Congress and VA to review the medical research linking these conditions to the contaminated water at Camp Lejeune and determine if VA’s presumptive list is accurate.
Thailand: When Agent Orange was sprayed on bases in Thailand during the war in Vietnam, it created yet another group of American service members who would later suffer from the effects of this poison. Currently, veterans must prove they worked on the perimeter of the base to which they were assigned to have their disability compensation claims considered under more streamlined presumptive rules.
U.S. forces in Thailand were supporting military operations in Vietnam and Agent Orange was used for the same purposes as in Vietnam. The spraying of vegetation allowed for the substance to go from a liquid state to one which is a mist that could float to other portions of the base. It is not incomprehensible for veterans in other parts of the base to have been exposed to Agent Orange. The VFW urges Congress to pass legislation to expand benefits to all veterans who served in Royal Thai bases where Agent Orange was used.
Single Gulf War Illness Disability Benefits Questionnaire Form: Unlike nearly all other service-connected conditions, Gulf War Illness (GWI) is intrinsically difficult to diagnose and treat. GWI has no clear and concise set of rules. In other words, no singular set of symptoms allows for an unmistakable diagnosis. GWI presents itself as a conglomeration of possible symptoms to which countless members of the general public with no military experience can also be subject. As such, Persian Gulf veterans have a steeper hill to climb in relating the symptoms to service –– the most critical link in establishing service-connection.
As a component of the VA disability compensation claims process and to better manage its workload, VA developed disability benefits questionnaire (DBQ) to assist in adjudicating claims. Since GWI is constituted by medically unexplained chronic illnesses, VA adjudicators often order examinations for each GWI symptom before considering the indicators that one illness is connected to the multiple symptoms.
The VFW is concerned that the current system of assigning separate DBQs for each symptom being claimed in association with GWI is the leading cause of high denial rates for GWI claims. VA must be required to provide additional testing and examinations deemed necessary by this examination. The VFW firmly believes that the creation of a singular DBQ for GWI claims would facilitate more timely and accurate consideration of disability compensation claims for veterans who suffer from GWI.
An overall lack of training for VHA medical staff who conduct medical examinations has also led to inaccurate processing of GWI disability compensation claims. To improve accuracy of claims and to ensure Persian Gulf War veterans receive accurate decisions, VA must require medical staff to complete periodic GWI-specific training before being authorized to conduct medical examinations for GWI disability compensation claims.
Expand the Definition of Persian Gulf War Veteran: Several scientific studies have found that veterans who have served in Afghanistan suffer from undiagnosed conditions at similar rates as those who have served in the Iraq. Additionally, veterans who served in support of Operation Desert Shield and Operation Desert Storm while stationed in Israel, Egypt, Turkey, Syria, and Jordan have also presented similar symptoms as veterans who served in Iraq. However, current law limits the definition of Persian Gulf War veteran to those who served on active duty in the U.S. Armed Forces in the Southwest Asia theater of operations, which is limited to Iraq, Kuwait, Saudi Arabia, the neutral zone between Iraq and Saudi Arabia, Bahrain, Qatar, the United Arab Emirates, Oman, Gulf of Aden, Gulf of Oman, and the waters of the Persian Gulf, the Arabian Sea, and the Red Sea.
As a result, veterans who have served in Afghanistan, Israel, Egypt, Turkey, Syria, and Jordan are denied access to presumptive disability compensation benefits afforded to Persian Gulf War veterans, despite evidence which shows such conditions are common among them. Furthermore, they are being considered Gulf War veterans for reporting and demographic purposes. Veterans who served in Israel, Egypt, Turkey, Syria, and Jordan in support of Operation Desert Shield and Operation Desert Storm are even eligible for the Southwest Asia Service Medal, but are denied access to streamlined disability compensation for disabilities they incurred during their service in Southwest Asia. Congress must expand the definition of Persian Gulf War veterans to include such veterans.
Expand VA Wartime Benefits to Early-Vietnam Veterans: On November 1, 1955, the U.S. Military Assistance Advisory Group (MAAG) Vietnam was officially established following the defeat of the French in Vietnam and the establishment of the 1954 Geneva accords. Records show that up to 10,000 U.S. military personnel served with MAAG-Vietnam and other U.S. military groups in Vietnam between November 1, 1955 and February 27, 1961. At least twelve US military personnel were awarded the Purple Heart in Vietnam prior to February 28, 1961 and ten U.S. military personnel were killed in Vietnam during the same time frame and are listed on the Vietnam Wall.
However, veterans who served in Vietnam from November 1, 1955 to February 27, 1961 are not considered wartime veterans and are ineligible for wartime VA benefits such as low-income wartime pensions. Congress must expand VA wartime benefits to include these veterans, known as Early Vietnam veterans.
Hearing and Tinnitus: Veterans who serve in combat are exposed to high levels of acoustic trauma. Many pre-service and discharge examinations, particularly for World War II and Korean War veterans, were usually accomplished with the highly inaccurate whispered-voice test which was discontinued many years ago. Many veterans in those cases were not afforded a comprehensive audiological examination upon entrance and/or discharge from military service. In the latest VBA Annual Report from September 2018, the most prevalent service-connected disabilities are hearing loss and tinnitus. In 2005, the Institute of Medicine (IOM) released a study that showed nearly all service members are exposed to acoustic trauma at some point during their military service and that many experience hearing loss and/or tinnitus as a result.
The VFW calls on Congress to establish presumptive benefits to combat veterans diagnosed with hearing loss or tinnitus. The Secretary of the VA must amend the Schedule for Rating Disabilities to provide a minimum compensable evaluation for any service-connected hearing loss for which a hearing aid is medically indicated.
Blast Injuries: While the face of war has changed over the past century, the nature of how they are fought has not. Now more than ever, we are seeing service members who are returning from combat with injuries as a result of their exposure to explosions. VA has been slow to provide a long-term solution that would address these injuries, despite the overwhelming evidence that suggests service members who are exposed to explosions or sustain concussions often times may experience delayed onset of symptoms ranging from headaches and cognitive impairments to even more severe neurological complications. The VFW calls on Congress to amend Title 38 to grant presumption of service connection for conditions associated with blast exposures.
Vocational Rehabilitation and Employment Services: Vocational rehabilitation for disabled veterans has been part of this nation’s commitment to veterans since Congress first established a system of veterans’ benefits upon entry of the United States into World War I in 1917. Today, Vocational Rehabilitation and Employment (VR&E) is charged with providing wounded, ill, and injured veterans with an array of services designed to enable them to obtain and maintain suitable and gainful employment. In the case of those veterans with more serious service-related disabilities, VR&E is authorized to provide independent living services.
Veterans are eligible for VR&E services and programs if their military discharge is other-than dishonorable and they have a VA service-connected disability rating of at least 10 percent, or a memorandum rating of 20 percent or more from VA. The VR&E program is also accessible to active duty military personnel expecting to be medically discharged with the requisite discharge and anticipated disability rating of at least 20 percent or more from DOD and VA.
The period of eligibility to apply for VR&E services cannot currently exceed 12 years from either the date of separation from active duty, or the date veterans are notified by VA of a service-connected disability rating. This 12-year application eligibility period can only be extended if a Vocational Rehabilitation Counselor determines a veteran has a serious employment handicap. Participants in VR&E also cannot exceed 48 months of entitlement. The 48-month period of entitlement, however, may also be extended in unique circumstances. The VFW calls on Congress to eliminate the 12-year delimiting period for VA Chapter 31 VR&E services to ensure disabled veterans with employment handicaps, including those who qualify for independent living services, qualify for VR&E services for the entirety of their employable lives. Congress must pass H.R. 444, the Reduce Unemployment for Veterans of All Ages Act of 2019.
VR&E’s incentive structure for veterans remains primarily aligned with education and training programs with no financial incentive for those seeking immediate employment. Considering the basic costs of living, veterans may be unable to wait until the completion of their program to generate some sort of income. They may be forced to leave the program prematurely simply to provide for themselves or their families. Child care vouchers for veterans who have families and are involved in VR&E could help these veterans remain in the program.
We ask Congress to change the eligibility requirements for the VR&E program to increase access to services while increasing subsistence allowances for veterans with dependents. Veterans’ service-connected illnesses and injuries are life-long consequences of service to our nation, and so too should veterans have the ability to utilize VR&E benefits throughout their lifetimes. Providing a payment to all VR&E users similar to the housing payments made to GI Bill recipients would allow for the disabled veterans utilizing this program to continue doing so without as much of a financial burden.
Finally, Congress must provide sufficient resources for VR&E to establish a maximum client-to-counselor standard of 125:1 or better, and explore new methodologies to formulate a proper client-to-counselor ratio based on the challenges associated with more severely disabled veterans. The VFW recommends changing reporting of the ratio to reflect the VAROs, instead of a nationwide client-to-counselor ratio. This will help address the needs of specific offices and more directly help veterans.
GI Bill: The 115th Congress was responsible for a great number of new benefits and programs, and one of the highlights was the passage of the Forever GI Bill. This incredible benefit removes the end date for future beneficiaries, adds benefits for STEM programs, and expands eligibility for Purple Heart recipients, families, and survivors. This was the largest expansion of the GI Bill since 2008, and the VFW is incredibly grateful for the overwhelming bipartisan support to make this happen.
While Congress did its job in passing the Forever GI Bill, VA struggled to do its job in implementing it. Many of the provisions in the Forever GI Bill were easily adopted, but implementing the Basic Allowance for Housing (BAH) changes proved much more difficult than originally expected. During the fall 2018 semester, almost 200,000 student veterans received delayed or incorrect BAH payments, leading to unnecessary hardships.
Proper implementation of programs like the Forever GI Bill is something that cannot be overlooked. The negative impact on student veterans’ lives along with the time and money wasted this past fall is unacceptable. VA must work with Congress and VSOs in order to make sure that benefits are implemented correctly and are being used properly by the beneficiaries. While we feel VA may be on the right track to correct this issue, we hope it has learned from its mistakes regarding collaboration and communication.
Transition Assistance: The VFW believes a proper well rounded transition from the military is one of the most important things our service members need in order to ease back into our society with minimal hardships. To that extent the VFW places great emphasis on ensuring veterans receive the best counseling and mentorship before they leave military service. Veterans who make smooth transition by properly utilizing the tools and programs available will face less uncertainty regarding their move from military to civilian life.
Today’s military has faced almost two decades of continuous war, and this extended time of conflict has shaped the experiences of all men and women who have worn the uniform defending our country. This experience of heightened conflict makes transitioning to the civilian world that much more important. Only a small percentage of Americans serve their country in the Armed Forces, so transitioning to the civilian world can bring with it its own set of trials and tribulations.
Transitioning service members face many hardships that include unemployment, financial difficulty, lack of purpose, separation anxiety, and many unknowns. In order to make this transition as easy as possible, there have been programs set in place to ease the hardship of this change. The VFW believes these programs are paramount in easing service members out of military life and into the civilian world.
The VFW views transition programs such as the Transition Assistance Program (TAP) and Soldier For Life (SFL) as key stepping stones in order to seamlessly transition to civilian life. The information provided to service members on VA benefits, financial management, higher education, and entrepreneurship are invaluable tools.
We are glad to see the five-day TAP classes was restructured last year, and we are eager to see what benefits the more efficient method of information delivery will bring. However, there were many other important provisions to reform TAP that were unfortunately left unfinished at the end of the 115th Congress, such as providing grants to organizations specializing in transition services, connecting transitioning service members with resources in their communities, and inclusion of accredited VSO’s into the formal TAP curriculum. Doing so would ensure veterans can succeed after leaving military service.
The VFW’s accredited service officers have been a resource for transitioning service members since 2001, and we continue to provide assistance to these men and women during this difficult time of change. We provide pre-discharge claims representation at 23 bases around the country and have been available for transitioning service members at the same time they receive their training in TAP. While the primary role for the VFW staff in the Benefits Delivery at Discharge (BDD) program is to help service members navigate their VA disability claims, they are also able to provide assistance for many other benefits and opportunities available.
Our BDD representatives offer guidance and information for many different transition opportunities that may not be covered in the TAP class. Our representatives are trained in education, employment, and financial management opportunities, and can be additional resources to the ones received during TAP classes. Service members who utilize additional resources such as BDD representatives are likely to face less unknown hurdles during transition.
Fourth Administration: VA is comprised of three administrations: National Cemetery Administration (NCA), Veterans Health Administration (VHA), and Veterans Benefits Administration (VBA). The VBA is in charge of, not only, compensation and pension but also the GI Bill, vocational rehabilitation, housing and business loans, and the broadly defined transition assistance program, which is shared with the Departments of Labor, Defense, and Homeland Security. Many of these programs are currently under the Office of Economic Opportunity (OEO) which is overseen by a Deputy Under Secretary. However, this position has been left vacant and that does not appear to change anytime soon.
Currently, the OEO programs are enmeshed with the myriad of entities that make up the VBA. Compensation, is the largest program and dominates the attention of the VBA which makes it difficult for the OEO programs to get adequate funding, specialized resources, and other prioritization. For example, while the VBA has been focused on the modernization and streamlining of the claims and appeals process, other important programs such as VR&E have seen a stagnation of resources and oversight. Between 2014 and 2018, VR&E participation has increased by approximately 17 percent while its funding has risen just under two percent despite a 2014 GAO report that recommended further performance and workload management improvements were needed.
This nation should have as much focus on the economic opportunities of our veterans as it does on their health care and benefits. In reality, not all veterans are seeking VA health care when they are discharged, they are not needing assistance from the NCA, and they are not all seeking disability compensation. However, the vast majority are looking for gainful employment and/or education. Congress should recognize the value of these programs by separating them into their own administration focused solely on their utilization and growth.
The VFW has long proposed that Congress enact legislation to separate from the VBA all programs currently in the OEO and create a fourth administration under VA with its own under secretary whose sole responsibility is the EO programs. This new Under Secretary for Economic Opportunity would refocus resources, provide a champion for these programs, and create that central point of contact for VSOs and Congress.
Homelessness: The VFW commends VA and the Department of Housing and Urban Development (HUD) for making significant strides toward ending veteran homelessness. The Annual Homeless Assessment Report census for 2018 shows promise in eliminating homelessness in the veteran population, with current numbers showing less than 40,000. This is a remarkable difference since 2010 when the number of homeless veterans was 74,087.
A homeless person is federally defined under the McKinney-Vento Act as an individual or family lacking fixed, regular and adequate nighttime residence, as well as those fleeing domestic violence or other dangerous or life-threatening conditions. VA is not precluded from assisting veterans who are temporarily living with friends or family –– commonly referred to as “couch surfing.” Yet, it has elected not to do so. This is particularly burdensome for women veterans who often do not feel safe due to violence or sexual assault in a homeless shelter, as well as for veterans with dependent children. The VFW urges Congress and VA to expand this definition so VA can provide more homeless benefits and services to homeless veterans who are couch surfing instead of living in a shelter or under a bridge.
Veterans with dependent children face diverse burdens with access to their earned benefits, including access to child care. Currently, VA has four pilot programs which offer on-site child care. These programs have been successful in increasing access to care and benefits. The VFW also encourages Congress to work with VA to provide more separate living arrangements for veterans with children and veterans who have survived sexual trauma. Congress and VA must work together to better understand that individuals face homelessness for different reasons, and their needs to overcome homelessness are equally unique.
VA’s homeless programs are holistic in nature and include medical, dental, and mental health services, as well as specialized programs for PTSD, sexual trauma, substance use disorder (SUD), and vocational rehabilitation. VA adopted a model of housing veterans first — rather than requiring them to be in recovery or treatment for mental health or SUDs prior to receiving housing assistance. Homeless prevention coordinators and peer mentors are imperative to the success of the program by helping veterans navigate the system and get the services they need. The VFW urges Congress and VA to consider increasing the use of peer specialists, particularly for veterans who are in recovery from SUDs and/or have experienced homelessness. Peers who have had similar experiences are often able to connect on a more personal level and can help homeless veterans overcome challenges they face in maintaining housing and sobriety.
For veterans on the verge of homelessness, there is currently little VA can do. Several benefits require veterans to be on the streets before they are deemed eligible. Many veterans who are on the verge of homelessness know they are being evicted, and nearly half of homeless veterans report temporarily staying with friends or family. This is why the VFW recommends Congress work with VA and the U.S. Department of Housing and Urban Development (HUD) to ensure veterans who are facing eviction or are temporarily staying in another person’s home are afforded the opportunity to obtain assistance. The VFW also strongly urges Congress to pass legislation that would provide cost-free child care to veterans living below the poverty line, or who are already homeless while using VA and DOL VETS employment training. If a veteran is not able to afford rent or is working to avoid homelessness, then it is impractical to assume the veteran can also afford child care services.
Veterans fortunate enough to obtain HUD-VA Supportive Housing (VASH) vouchers also face difficulties. VFW service officers have reported in various cities that homeless veterans sometimes prefer sleeping under a bridge rather than living in the unsafe neighborhoods for which their vouchers are eligible. The VFW urges Congress, VA, and HUD to work together with local VA facilities to ensure HUD-VASH vouchers put veterans in safe and secure housing.
Electronic Health Record System, Modernization: The VFW was pleased VA elected to adopt the same electronic health care record (EHR) system as DOD, putting an end to the saga of not being able to efficiently integrate military treatment records into veterans’ treatment plans. This plan will greatly improve the delivery of care to ill and injured veterans, and ensure truly integrated care as service members transition from the Military Health Care System to to the VA health care system.
Additionally, VA must ensure clinicians are driving the implementation effort so VA can provide a truly seamless transition for our service members and our veterans, while ensuring the best clinical outcome for veterans.
Nursing Homes: VA eligibility for nursing home care is limited to veterans with a service-connected disability rating of 70 percent or higher, or for those seeking care at a nursing home for conditions related to their service-connected disabilities. Nursing home care is the only form of long-term service and support that is not included in the health benefits package –– which VA acknowledges in their own statements is inconsistent with principles of medical practice and does not support continuity of care veterans are supposed to receive at VA. Congress must pass legislation to amend VA’s health care benefits package to include nursing home, just as all veterans are eligible to receive home and community-based services.
Preventive Medicine & Services: The VA formulary currently carries all categories of pharmaceuticals deemed preventive by the U.S. Preventive Services Task Force. However, VA is exempt from requirements to provide preventive care and services without cost shares.
Cost is a significant barrier for veterans who use VA health care, whom have been found to have a lower income on average than veterans who do not use VA health care. There are currently 11 categories of preventive medications found to be effective by the U.S. Preventive Services Task Force, such as prescribing aspirin to lower the risk of cardiovascular disease. Cardiovascular disease is the number one cause of death in the United States and is highly prevalent among the veteran population. Additionally, folic acid is recommended for pregnant women to prevent neural tube defects. It is unjust to require women veterans to pay for the cost of preventive medication to prevent such birth defects. Vitamin D is another preventive medicine which is often prescribed to prevent bone fractures, which benefits TBI patients with hindbrain injuries. There is also breast cancer prevention medication which is useful not just for individuals with a family medical history of breast cancer, but for Camp Lejeune toxic water survivors who have been found to suffer from increased rates of breast cancer. These pharmaceuticals have been found to not just prevent possible disease, and to be cost-saving.
The VFW calls on Congress to swiftly pass the Veterans Preventive Health Coverage Fairness Act, which would eliminate this inequity and ensure veterans have access to lifesaving preventive medicine.
Health Disparities for Minorities & LGBT: According to VHA’s Offices of Patient Care Services and Health Equity, an estimated one million LGBT veterans face unique challenges to accessing the quality health care they have earned through their service. As a result, LGBT veterans experience overall lower health statuses in both clinical settings and their personal health. LGBT individuals also experience mental health problems and death by suicide at a higher rate than their heterosexual counterparts. Other high-risk conditions for LGBT veterans include heart disease for gay and bisexual men, as well as intimate partner violence, obesity, and early death from cancer for lesbian and bisexual women. Older LGBT veterans are less likely to receive care from adult children and may experience discrimination in nursing homes or community living centers, or live in fear of such scenarios if their sexual orientation or gender identity is not publicly known. These health disparities also change and worsen for LGBT veterans who are racial or ethnic minorities. Just as post-9/11 veterans face different health care challenges than those who served in the Vietnam War, and just as women veterans face different health care challenges than their male counterparts, LGBT veterans have specific, medically necessary needs that must be met.
Since VA’s first directive for transgender veterans in 2011, the number of veterans enrolling in VHA who identify as transgender has been steadily increasing. To assure providers are able to deliver the highest quality of care to transgender veterans, VA’s Health Equity Action Plan (HEAP) was established in 2016 to undertake, advance, and achieve equitable health for all veterans. The action plan includes cultural and linguistic competency, as well as data, research, and evaluation.
To improve cultural competency, VA suggested improving the diversity of its health-related workforce. While this recommendation was made in 2016 as part of HEAP, there is no current data available regarding VA’s LGBT staffing numbers to note any areas of improvement in diversifying staff. The remaining recommendations are supportive of the inclusion of educational curriculum in training, and partnerships to improve inclusion of cultural competency in training and activities. Yet, these recommendations have not been addressed in internal directives, and there are still no requirements of formal training for medical staff.
VA must ensure the National LGBT Health Program positions are staffed. This includes the national program director position at the VA Central Office, every LGBT Veterans Integrated Service Networks (VISN) lead, and all LGBT veteran care coordinators. The VFW urges congressional oversight to assure these positions are filled, and the Center for Minority Veterans to be authorized to work with LGBT veterans.
HEAP also calls for improving data availability and coordination, utilization, and diffusion of research and evaluation outcomes. Yet, the only National Veteran Health Equity report published in 2016 details care for veterans receiving care in FY 2013. This is the most recent data available based on race/ethnicity, gender, age, geography, and mental health status. Having such minimal and outdated data makes identifying health inequities and systematic failures difficult for LGBT veterans who deserve the same quality of care that all veterans have earned through their service.
One area with timely data is VA pharmacies. Since 2012, when the U.S. Food and Drug Administration approved the first drug to reduce the risk of HIV infection in uninfected individuals who are at high risk of HIV infection, VA has annually increased the Pre-Exposure Prophylaxis (PrEP) prescription rates. In FY 2018, VA pharmacies filled 84,425 30-day equivalent prescriptions. While these prescription rates seem high, they average just over 7,000 per month and are not nearly high enough for the current population of LGBT veterans. This is why VA must work to conduct a strategic outreach campaign to educate LGBT veterans who are at increased risk of contracting HIV compared to their heterosexual counterparts, that PrEP is available at VA pharmacies.
According to VA’s Office of Research and Development, health care is distributed unevenly in the United States. Minority populations often receive less care or care of lesser quality compared to their Caucasian peers.
The minority veteran population makes up 22 percent of all veterans and accounts for over 34 percent of the women veteran population. Health disparities faced by racial and ethnic minorities compared to Caucasians include higher rates of chronic illnesses such as diabetes and high blood pressure, higher rates of cancer, and mental illness diagnosis.
There are no simple answers to these disparities. These disparities are prevalent across the entire American health care ecosystem and are still demonstrated within VA, where many financial barriers to receiving care are minimized. With this in mind, Congress must commit to providing racial and ethnic minority veterans with high-quality care in an equitable manner. To do this, research must be conducted and analyzed on how to eliminate racial and ethnic disparities. Recent research found health disparities among racial and ethnic minority veterans for arthritis and pain management, cancer treatment, cardiovascular disease, diabetes, HIV and Hepatitis C, mental health and substance abuse, rehabilitative and palliative care, dental procedures, use of new medical technology, preventive and ambulatory care, among others.VA must also be able to conduct outreach to those who are not actively trying to obtain health care so they can be brought into the system for care. The need is evident as studies published by the American Journal of Public Health have found mortality rates are higher for black veterans.
Solving these health disparities will not come with a straightforward or simple solution. While access to health care is certainly a major piece of this puzzle, other factors – including income, life experiences, education, support, and social context are all components of why these disparities exist. VA will not be able to address racial and ethnic health disparities without a holistic approach.
Burial Benefits: The cost of funeral expenses in the private sector have increased nearly seven-fold since 2001, but VA benefits to cover such costs have failed to keep pace with inflation. The VFW urges Congress to ensure the loved ones of veterans who do not have access to a state or national veterans cemetery within 75 miles are not required to accumulate debt to provide their loved ones a final resting place that honors their sacrifice to our nation.
The VFW calls on Congress to pass H. R.497, the Burial Rights for America’s Veterans’ Efforts (BRAVE) Act, which would increase the funeral and burial benefit for eligible veterans. This important bill would also ensure burial benefits are indexed for inflation.
Mare Island Naval Cemetery: The U.S. Navy used the Mare Island Cemetery as the final resting place for more than 800 veterans, including three Medal of Honor recipients. This cemetery is in disrepair and the VFW will never stand by as the final resting place of veterans is neglected and forgotten. The VFW strongly supports passage of H.R. 570 or S. 127, which would transfer ownership of Mare Island Naval Cemetery to VA.
VA Construction and Infrastructure Review: For more than 100 years, the government’s solution to provide health care for our military veterans has been to build, manage, and maintain a network of hospitals across the nation. This model allows VA to deliver care at 1,753 facilities, but has left it with more than 5,600 buildings and 34,000 acres, many of which are past their building lifecycle. Many of these facilities need to be replaced, some need to be disposed of, others need to be upgraded and expanded. All buildings being utilized need to be regularly maintained. The current process to manage this network of facilities is the Strategic Capital Investment Plan (SCIP). SCIP identifies VA’s current and projected gaps in access, utilization, condition, and safety, in order of priority.
The VFW calls on VA to immediately begin a review of its capital Infrastructure priority lists and set in place a plan to work through the list of current projects within ten years, regardless of the outcome of the upcoming Asset and Infrastructure Review mandated by the VA MISSION Act. Once the reviewed priority list is established, VA needs to ensure all seismic and life safety issues are placed at the top of the SCIP list and remain at the top until they are rectified. Having seismic deficiencies on the SCIP list year after year is unacceptable and could lead to catastrophic events if left unresolved.
A key component of the VA MISSION Act is to conduct an Asset Infrastructure Review to determine how VA physical assets should be best utilized. Conducting market assessments in order to right size the physical footprint of VA is an incredibly important and complicated task, and we insist that VA be as inclusive and transparent throughout the entire process so the correct outcome is achieved. Inclusion of veteran groups and key stakeholders is vital to make sure that VA gets it right the first time.
VA also needs to prioritize non-recurring maintenance (NRM) as these oftentimes represent critical deficiencies which directly affect patient safety on a daily basis. For example, the need for heating and cooling system repairs, or generator upgrades may not immediately stand out as critical, but failures of these systems could lead to life safety issues. Additionally, deferring regular maintenance issues and upgrades is typically not prudent as this often exacerbates problems which necessitates more costly future remedies.
The VFW recommends shifting VA’s construction model to an Integrated Design Build (IDB) model for its construction projects in order to maximize efficiency and cost savings. This will allow the VA to shorten the overall length of major construction projects, by overlapping the three phases of the project.
The VFW also recommends for VA to explore using a more standardized modular design and building model. There always needs to be room for different buildings or layouts to be utilized in individual cases, but moving towards a standardized layout and construction could lead to a faster and more streamlined building of facilities. There is no need for VA facilities to be designed based on aesthetics. Facilities should be built with the patients in mind, meaning getting from groundbreaking to ribbon cutting in the most effective and simplified manner possible. The example of the Rocky Mountain Regional VA Medical Center in Denver must not be repeated. The impractical design never had the patients in mind and this type of mistake can be corrected by simplifying the design and build of medical facilities.
Concurrent Receipt & SBP/DIC: The VFW has long argued that retired pay and VA service-connected disability compensation are fundamentally different benefits, earned for different reasons. Military retired pay is earned by 20 or more years of service in the United States Armed Forces, allowing retirees to maintain their standard of living while attempting to enter the civilian job market for the first time in the middle of their prime working years.
Service-connected disability compensation is a benefit meant to supplant a veteran’s lost earning potential as a result of the disabilities he or she incurred while in service. However, military retirees who are less than 50 percent service-connected disabled are required to offset their retiree pay with the amount of VA disability compensation they receive. Congress must pass H.R. 303 or S. 208, the Retired Pay Restoration Act, which would enable disabled retirees to concurrently receive the retirement pay and VA disability compensation they have earned and deserve, without offset.
Since military retirement pay cannot be passed on to a survivor, military retirees opt to pay for the Survivor Benefit Plan (SBP), which is an insurance that helps provide for their surviving family members. The survivors of military retirees who die from a service-connected injury are unjustly forced to endure a dollar-for-dollar offset of their SBP payments and Dependency and Indemnity Compensation, which is granted to survivors of the brave men and women who make the ultimate sacrifice or die from wounds they sustained in service to our nation. Congress must pass H.R. 553, the Military Surviving Spouses Equity Act, which would honor the sacrifices of our nation’s heroes by ensuring their survivors maintain a modest quality of life, without having to unjustly offset their benefits.
The only purpose for these two offsets is to balance the federal budget on the backs of America’s disabled veterans and their survivors. They are different benefits paid by two separate government entities for separate reasons.
POW/MIA Full Accounting Mission: The VFW has been intimately involved in the Full Accounting Mission since as early as 1929 when we conducted a mission financed by Congress and approved by the Soviet Union to recover the bodies of 128 American war dead who died in North Russia fighting the Bolsheviks after the World War I Armistice was signed.
Through the ensuing decades of new conflicts, we remain the only veterans' organization to send our senior leaders to Southeast Asia every year since 1991, to Russia since 2004, and to China since 2008, in order to help American researchers gain deeper access to foreign military archives. We were also the only organization to engage with President Trump regarding the return of Korean War remains prior to his successful Singapore Summit last year. Our actions resulted in the transfer of 55 boxes of remains by the DPRK, and opened the door for Joint Field Activities to resume in North Korea in the near future.
The fullest possible Accounting Mission remains a top priority for the VFW. With more than 82,000 U.S. service members still unaccounted for globally, the VFW will continue to advocate for full mission funding and personnel staffing for the Defense POW/MIA Accounting Agency, as well as its supporting agencies, such as the Armed Forces DNA Identification lab and the military service casualty offices.
Locating, identifying, and recovering the remains of those who paid the ultimate sacrifice in the service of our country from conflicts spanning nearly 80 years is a difficult and hazardous mission, but it is one of the most the important obligations that that we have as a country. It is a mission and it is a promise to those serving in uniform today that no matter what, we will travel to the ends of the Earth to return you home to your families. As a veteran who served in Korea, I am honored to have played a role in reuniting fallen veterans whose remains remained behind enemy lines in North Korea with their loved ones.
I know supporting this mission is something we can all agree on, and it is why we urge Congress to ensure this important mission is able to continue in perpetuity, and regardless of any lapse in government funding. It is insufferable that recovery missions or Joint-Field Activities, which take an enormous amount of time, energy and resources to plan and must be conducted during certain times of the year, are suspended simply because Congress cannot do its job.
Finally, we were grateful to see the return of 55 boxes of remains back to the U.S. last year by the Democratic People's Republic of Korea (DPRK). Some see DPRK’s decision to do so as nothing more than an empty gesture or one meant to only placate. However, to the families of the 5,200 service members who never came home from the Korean War, those boxes represent hope and closure. It is for this reason that we also seek your support to increase the necessary resources to expand recovery operations into North Korea and to support the remains recovery mission in DPRK as fully as possible.